Parenchymal lung disease, a complex condition affecting the delicate lung tissue, unveils a captivating medical narrative. Its diverse forms, intriguing causes, and intricate management strategies paint a multifaceted picture that demands our attention.
From understanding the underlying mechanisms to exploring the latest therapeutic advancements, this comprehensive guide delves into the enigmatic world of parenchymal lung disease, unraveling its complexities with clarity and precision.
Definition and Overview of Parenchymal Lung Disease
Parenchymal lung disease (PLD) refers to a group of conditions that primarily affect the functional tissues of the lungs, known as the parenchyma. The parenchyma is responsible for gas exchange, the vital process of oxygen uptake and carbon dioxide removal.
When the parenchyma is damaged or diseased, it can impair the lungs’ ability to perform this essential function.PLD can be classified into two main types:
- Restrictive lung diseases:These diseases reduce the lungs’ ability to expand fully, limiting the amount of air that can be inhaled. Examples include interstitial fibrosis, sarcoidosis, and asbestosis.
- Obstructive lung diseases:These diseases narrow the airways, making it difficult to exhale air. Examples include chronic obstructive pulmonary disease (COPD), asthma, and bronchiectasis.
Causes and Risk Factors: Parenchymal Lung Disease
Parenchymal lung diseases can arise from various causes, including:
Infections
Bacterial, viral, fungal, and parasitic infections can cause parenchymal lung disease, such as pneumonia, tuberculosis, and histoplasmosis.
Environmental factors
Exposure to pollutants, such as cigarette smoke, air pollution, and occupational hazards like silica and asbestos, can damage lung tissue.
Autoimmune disorders
Conditions like sarcoidosis, rheumatoid arthritis, and systemic lupus erythematosus can trigger inflammation in the lungs, leading to parenchymal lung disease.
Genetic disorders
Certain genetic mutations can cause inherited lung diseases, such as cystic fibrosis and alpha-1 antitrypsin deficiency.Risk factors associated with parenchymal lung diseases include:
Smoking
Cigarette smoking is a major risk factor for developing chronic obstructive pulmonary disease (COPD) and other parenchymal lung diseases.
Exposure to air pollution
Prolonged exposure to high levels of air pollution can increase the risk of lung damage and disease.
Occupational hazards
Individuals exposed to certain occupational hazards, such as silica, asbestos, and other chemicals, have an increased risk of developing parenchymal lung disease.
Family history
People with a family history of lung disease may have an increased risk of developing the condition.
Age
The risk of parenchymal lung disease increases with age.
Symptoms and Clinical Presentation
Parenchymal lung diseases present with a range of symptoms, including:
- Shortness of breath:This is a common symptom of parenchymal lung diseases, especially during exertion or exercise.
- Cough:A persistent cough is another common symptom, which may be dry or productive.
- Wheezing:This is a whistling sound during breathing, which indicates airway narrowing.
- Chest pain:This can be a sharp or stabbing pain, which is often worse with coughing or deep breathing.
- Fatigue:People with parenchymal lung diseases often experience fatigue, as the lungs work harder to breathe.
In addition to these common symptoms, parenchymal lung diseases can also present with more specific clinical features, depending on the underlying cause. For example, idiopathic pulmonary fibrosis (IPF) can cause a characteristic “crackling” sound in the lungs, while sarcoidosis can lead to skin rashes and joint pain.
Diagnosis and Imaging Findings
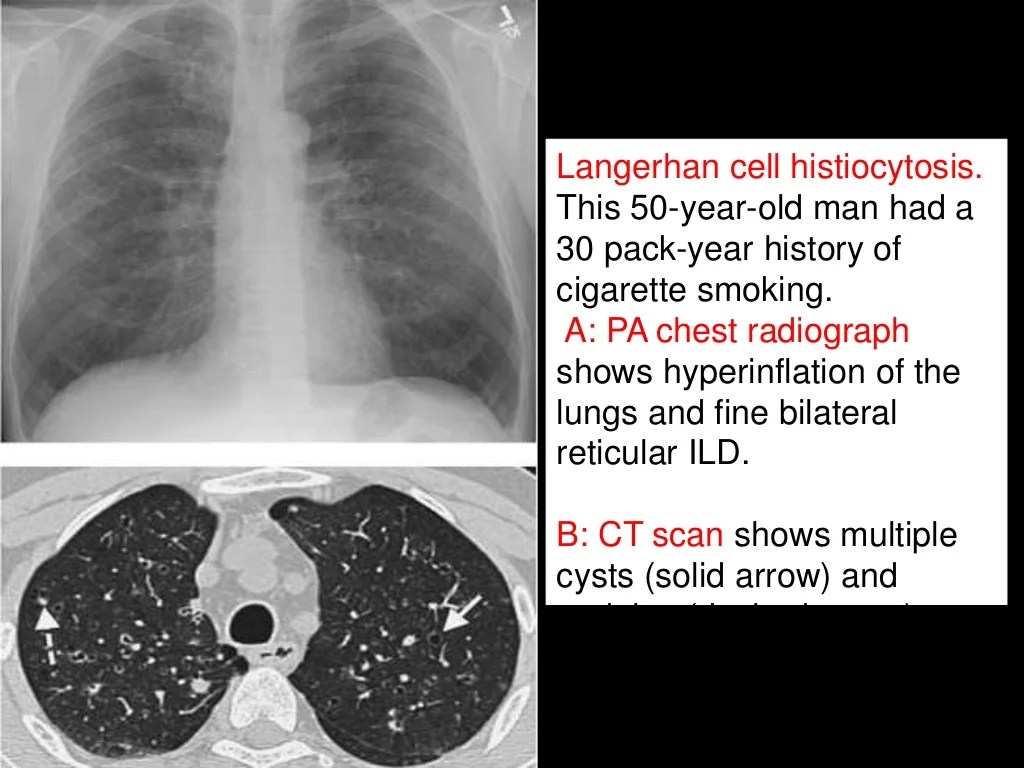
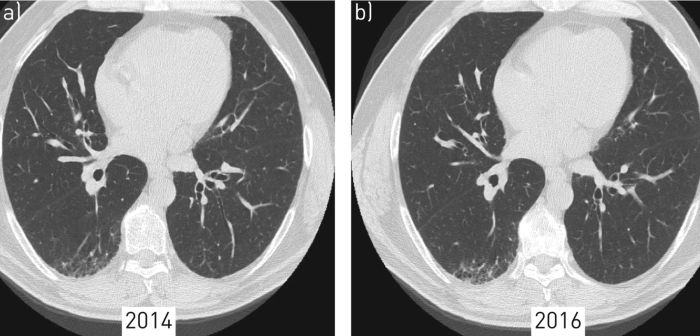
Diagnosis of parenchymal lung diseases involves a combination of medical history, physical examination, and diagnostic tests. Imaging findings play a crucial role in confirming the diagnosis and determining the extent of lung involvement.
Diagnostic Tests
- Pulmonary function tests (PFTs)measure lung function and detect abnormalities in airflow and gas exchange.
- Chest X-rayprovides a general view of the lungs and can reveal changes in lung density or structure.
- Computed tomography (CT) scancreates detailed cross-sectional images of the lungs, allowing for precise evaluation of lung parenchyma and airways.
- Magnetic resonance imaging (MRI)provides detailed images of the lungs and can be useful in differentiating between different types of lung diseases.
- Bronchoscopyinvolves inserting a thin, flexible tube into the lungs to visualize the airways and collect samples for further analysis.
Imaging Findings
Imaging findings associated with parenchymal lung diseases vary depending on the underlying cause and severity of the condition. Common findings include:
- Ground-glass opacities (GGOs): Hazy areas of increased lung density, often associated with inflammation or fibrosis.
- Consolidation: Areas of solid lung tissue, indicating fluid or inflammatory infiltrate filling the air spaces.
- Reticular opacities: Fine lines or networks of increased density, indicating thickening of the lung interstitium.
- Nodules: Small, round areas of increased density, representing areas of inflammation, infection, or tumor.
- Honeycombing: A pattern of small, cystic air spaces, indicating severe lung damage and fibrosis.
Histopathology and Pathology
The histopathological features of parenchymal lung diseases vary depending on the specific disease process. However, some common features include:
- Interstitial fibrosis:This is the most common histopathological feature of parenchymal lung diseases. It is characterized by the presence of excess collagen and other extracellular matrix proteins in the lung tissue.
- Alveolar damage:This can occur in various forms, such as alveolar collapse, emphysema, or hemorrhage.
- Inflammatory cell infiltration:This is a common feature of parenchymal lung diseases, and the type of inflammatory cells present can vary depending on the specific disease process.
The pathological mechanisms underlying parenchymal lung diseases are also varied. Some of the most common mechanisms include:
- Immune dysregulation:This can lead to the development of autoimmune diseases that target the lung tissue.
- Exposure to toxins or environmental pollutants:These can damage the lung tissue and lead to the development of parenchymal lung diseases.
- Genetic mutations:These can lead to the development of inherited parenchymal lung diseases.
Treatment and Management
The treatment and management of parenchymal lung diseases depend on the underlying cause and the severity of the condition. The primary goal of treatment is to relieve symptoms, improve lung function, and prevent complications.
Medications
- Bronchodilators: These medications relax the muscles in the airways, making it easier to breathe.
- Inhaled corticosteroids: These medications reduce inflammation in the airways.
- Antibiotics: These medications are used to treat bacterial infections that may contribute to parenchymal lung disease.
- Antifungal medications: These medications are used to treat fungal infections that may contribute to parenchymal lung disease.
Oxygen Therapy
Oxygen therapy is used to increase the amount of oxygen in the blood. This can help improve lung function and relieve symptoms.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a program of exercises and education that can help improve lung function and quality of life.
Lung Transplantation
In severe cases of parenchymal lung disease, lung transplantation may be an option. This is a major surgery that involves replacing the damaged lungs with healthy lungs from a donor.
Prognosis and Complications
The prognosis of parenchymal lung diseases varies depending on the underlying cause, severity, and individual patient factors. In general, early diagnosis and treatment can improve the prognosis and prevent complications.
Potential complications associated with parenchymal lung diseases include:
Respiratory Failure
- Severe parenchymal lung diseases can lead to respiratory failure, a life-threatening condition in which the lungs are unable to provide adequate oxygen to the body.
- Respiratory failure may require mechanical ventilation or other supportive measures to assist breathing.
Pulmonary Hypertension
- Parenchymal lung diseases can increase the pressure in the pulmonary arteries, leading to pulmonary hypertension.
- Pulmonary hypertension can damage the heart and other organs over time.
Cor Pulmonale
- Cor pulmonale is a condition in which the right side of the heart becomes enlarged and weakened due to pulmonary hypertension.
- Cor pulmonale can lead to heart failure and other complications.
Other Complications
- Parenchymal lung diseases can also increase the risk of infections, blood clots, and other health problems.
- Early diagnosis and treatment can help prevent or manage these complications.
Differential Diagnosis
Differentiating parenchymal lung diseases from other conditions is crucial for accurate diagnosis and management. Key considerations include:
Infectious Diseases:Pneumonia, tuberculosis, and fungal infections can mimic parenchymal lung diseases, causing inflammation and interstitial thickening.
Imaging Findings
- Pneumonia: Consolidation and air bronchograms
- Tuberculosis: Nodules, cavities, and hilar lymphadenopathy
- Fungal infections: Halo sign on CT scan
Clinical Presentation, Parenchymal lung disease
- Infectious diseases often present with fever, cough, and sputum production
- Parenchymal lung diseases may have a more insidious onset with dyspnea and cough
Vascular Diseases:Pulmonary embolism and pulmonary hypertension can cause pulmonary edema and interstitial thickening.
Imaging Findings
- Pulmonary embolism: Wedge-shaped opacities
- Pulmonary hypertension: Kerley B lines and dilated pulmonary arteries
Clinical Presentation, Parenchymal lung disease
- Vascular diseases typically present with sudden onset of dyspnea and chest pain
- Parenchymal lung diseases usually have a more gradual onset
Airway Diseases:Asthma and chronic obstructive pulmonary disease (COPD) can cause airway obstruction and inflammation, leading to parenchymal changes.
Imaging Findings
- Asthma: Air trapping and bronchial wall thickening
- COPD: Emphysema and bronchiectasis
Clinical Presentation, Parenchymal lung disease
- Airway diseases typically cause wheezing, shortness of breath, and coughing
- Parenchymal lung diseases may present with similar symptoms, but often with a more insidious onset
Case Studies and Examples
Case studies of patients with parenchymal lung diseases provide valuable insights into the presentation, diagnosis, and management of these conditions. By examining real-world examples, clinicians can gain a deeper understanding of the complexities of these diseases and improve their ability to provide effective care.
Interpreting and Analyzing Case Studies
When interpreting and analyzing case studies, it is important to consider the following factors:
Patient demographics
Age, sex, ethnicity, and occupation can provide clues to the underlying cause of the disease.
Clinical presentation
The patient’s symptoms, physical examination findings, and medical history can help narrow down the differential diagnosis.
Diagnostic testing
The results of imaging studies, pulmonary function tests, and biopsies can provide essential information for diagnosis and staging.
Treatment and management
The patient’s response to treatment can provide insights into the effectiveness of different therapeutic approaches.
Prognosis and complications
The patient’s long-term outcomes and any complications that arise can help clinicians better understand the natural history of the disease and its potential impact on the patient’s quality of life.By carefully analyzing these factors, clinicians can gain a comprehensive understanding of the patient’s condition and develop an individualized treatment plan that is tailored to their specific needs.
Emerging Therapies and Research
Research into parenchymal lung diseases is ongoing, and several emerging therapies are showing promise in treating these conditions. These include:
- Targeted therapies:These drugs target specific molecules or pathways that are involved in the development of parenchymal lung diseases. For example, tyrosine kinase inhibitors (TKIs) have been shown to be effective in treating idiopathic pulmonary fibrosis (IPF).
- Immunomodulatory therapies:These drugs suppress the immune system to reduce inflammation in the lungs. They are being investigated as a potential treatment for a variety of parenchymal lung diseases, including IPF and sarcoidosis.
- Stem cell therapy:Stem cells have the potential to repair damaged lung tissue. They are being studied as a potential treatment for a variety of parenchymal lung diseases, including IPF and chronic obstructive pulmonary disease (COPD).
In addition to these emerging therapies, researchers are also investigating the use of new imaging techniques to diagnose and monitor parenchymal lung diseases. These techniques include:
- High-resolution computed tomography (HRCT):HRCT is a type of CT scan that provides detailed images of the lungs. It is used to diagnose and monitor a variety of parenchymal lung diseases, including IPF and sarcoidosis.
- Magnetic resonance imaging (MRI):MRI is a type of imaging that uses magnets and radio waves to create images of the body. It is being investigated as a potential tool for diagnosing and monitoring parenchymal lung diseases.
These emerging therapies and research findings offer hope for improved outcomes for patients with parenchymal lung diseases.
Ultimate Conclusion
Parenchymal lung disease stands as a testament to the intricate tapestry of human health. Its myriad manifestations, from subtle symptoms to life-altering complications, underscore the importance of early detection and prompt intervention. Through ongoing research and the relentless pursuit of knowledge, we continue to unravel the enigmas of this enigmatic condition, paving the way for improved outcomes and a brighter future for those affected.
Question & Answer Hub
What is the most common symptom of parenchymal lung disease?
Shortness of breath, particularly during exertion, is a hallmark symptom.
What causes parenchymal lung disease?
Causes vary widely, including infections, autoimmune disorders, environmental exposures, and genetic factors.
How is parenchymal lung disease diagnosed?
Diagnosis involves a combination of physical examination, imaging tests, and lung function assessments.
What are the treatment options for parenchymal lung disease?
Treatment depends on the underlying cause and may include medications, oxygen therapy, and in severe cases, lung transplantation.
What is the prognosis for parenchymal lung disease?
Prognosis varies depending on the type and severity of the disease, but early diagnosis and treatment can significantly improve outcomes.